The Pfizer and Moderna Vaccines
Column #273
Chinese author Wan Quan made the first reference to a smallpox inoculation in his “Douzhen xinfa” published in 1549. The first modern smallpox vaccine was developed in 1796. These developments were really big advancements because smallpox had about a 30% fatality rate. Because of vaccinations, smallpox was eventually eradicated and the vaccine is no longer administered. Interestingly, the World Health Organization has posted a report by John Ioannidis that projects the COVID-19 fatality rate to be 0.23%.1 2
During the twentieth century a wide variety of vaccines for viruses were developed and improved upon. To this day advancements are proceeding, but the special urgency caused by COVID-19 has ramped up development significantly. The urgent need for vaccines prompted an international response that had more than 120 candidate SARS-CoV-2 vaccines in development by June of 2020. The first ones to gain the most attention rounding the bend for the homestretch were the Pfizer and Moderna vaccines. Their success has caused considerable excitement and a little controversy at the same time.
The new Pfizer and Moderna vaccines seem to be exceptionally effective, but in order to develop them in a few months rather than over many years, their vaccines are utilizing new technology. All the many vaccines in use today are very traditional, but not the new ones that are being developed. That’s because the new ones are “synthetic messenger RNA” (mRNA) vaccines. So, this begs the question, where are we in the vaccine battle with COVID-19?
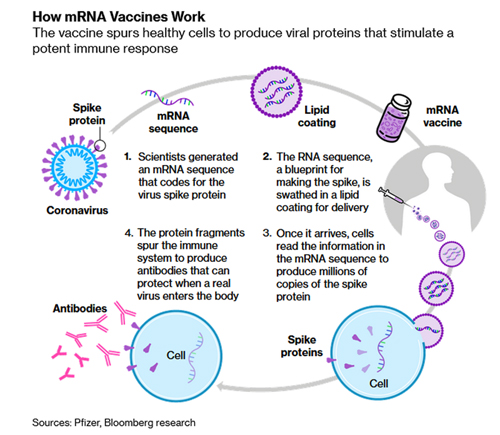
What I find interesting is that unwanted side-effects, which were expected to be worse than what would normally follow the administration of a flu vaccine, appear to be very mild. Potential side-effects are a concern because these new mRNA vaccines are the first of their kind and they don't work like any other previously approved vaccines. Normally vaccines use injected dead or weakened viral genetic material to provoke an immune response.
The new mRNA approach is designed to transform the body’s own cells into vaccine-making factories. The vaccines instruct cells to make copies of the spike protein of the coronavirus, stimulating the creation of protective antibodies.
For example, Moderna’s new mRNA-1273 vaccine consists of a strand of mRNA that tells the body to produce the “spike protein” the coronavirus uses to latch on to human cells. We’re told that this strand functions like one side of a zipper: the “teeth” are a sequence of chemical letters that cells read to produce the 1,273 amino acids comprising the famous protein “spikes” that the virus uses to latch on to human cells. The expectation is that the vaccine will start producing the proteins soon after injection, stimulating the immune system to react and build up protective antibodies against them.
Here is a graphic from Bloomberg illustrating how the mRNA vaccines work.
 The findings as released so far indicate that Pfizer's vaccine will be 95% effective and Moderna's will be 94.5% effective. Moderna’s data indicates that side effects were generally short-lived and there were no significant safety concerns. There were also no serious Covid-19 cases developed among trial participants who got the vaccine.
The findings as released so far indicate that Pfizer's vaccine will be 95% effective and Moderna's will be 94.5% effective. Moderna’s data indicates that side effects were generally short-lived and there were no significant safety concerns. There were also no serious Covid-19 cases developed among trial participants who got the vaccine.
The funding for the development of the two vaccines was different. Moderna received $955 million from the U.S. Operation Warp Speed program. Pfizer didn’t receive any federal funding, but its partner BioNTech got the equivalent of $444 million in German government assistance. Pfizer did strike a supply agreement with the U.S. worth nearly $2 billion and the U.S. agreed to pay up to $1.53 billion to purchase a supply of the Moderna shot.
After the vaccines are approved, the next big challenge is to immunize hundreds of millions of people. Storage and distribution of such a huge quantity of these vaccines are complex. Pfizer’s vaccine must be stored ultra-cold until a few days before it is used, but can be kept at refrigerator temperatures for as many as five days. Moderna says it vaccine can be stored in regular freezers over the longer term and then kept stable at refrigerator temperatures for 30 days.
There’s no question that the mRNA vaccines are a totally new technology. They are showing surprisingly good results in the short term, but of course there is no long-term data. Therefore, many questions remain about their long-term efficacy and side effects.
The U.S. government’s Operation Warp Speed program, which is underwriting both of these new mRNA vaccines, brought about a worrying response from Peter Hotez, an authority on vaccines and dean of the National School of Tropical Medicine at Baylor College of Medicine. He said “I worry about innovation at the expense of practicality when it is weighted toward technology platforms that have never made it to licensure before.”3
So, this is another example of scientists not being on the same page. It’s the same with mask wearing, shutdowns, the validity of tests, cattle grazing grasslands, mankind’s influence on the world’s temperature, forest management, and many other aspects of life. Science isn’t always fact. Often it has something to do with the beholder. As for these new vaccines, time will tell. They may be the medical innovation of this century.
In the interim, while waiting for a vaccine, I believe it’s imperative that everyone focus on improving their own immunity with proven, perfectly safe approaches that have stood the test of time.
The science is clear. To optimize immune system function avoid the sugars, carbohydrates, high Omega-6 sources, and strive for a 1:1 balance of Omega-6 to Omega-3 essential fatty acids (EFAs) in the diet. It works for all ages and most significantly for folks more than 40 years old. Health wise, many people start hitting the wall in their forties. By their 70s they’re a mess and that’s why they’re most vulnerable to COVID-19.4
I want to add that the best foods are nutrient dense and diverse, with ratios close to 1:1 for EFAs, that are also low glycemic. Yes, grass-fed meats, Omega-3 meats, wild-caught seafood, the dark green leafy vegetables, and many other vegetables such as squashes and beans are excellent selections. Foods from seeds, nuts, grains, most oils, and grain-fed meats that are high in Omega-6 EFAs should be avoided whenever possible.5
To your health.
Ted Slanker
Ted Slanker has been reporting on the fundamentals of nutritional research in publications, television and radio appearances, and at conferences since 1999. He condenses complex studies into the basics required for health and well-being. His eBook, The Real Diet of Man, is available online.
1. The Smallpox Vaccine Was First from Wikipedia
2. Infection Fatality Rate of COVID-19 Inferred from Seroprevalence Data by John P A Ioannidis from World Health Organization
3. The story of mRNA: How a once-dismissed idea became a leading technology in the Covid vaccine race by Damian Garde from StatNews
4. Omega-3 Fatty Acids in Inflammation and Autoimmune Diseases by Artemis P. Simopoulos
5. Food Analysis: EFA, Protein to Fat, Net Carbs, Sugar, and Nutrient Load by Ted Slanker