Omega-3 and Interferon
The people with the highest risk of a severe infection or death from COVID-19 are elderly males with underlying medical conditions. Yet some elderly males don’t even experience serious symptoms. That’s because several factors influence severity, including pre-existing levels of inflammation, natural immunity levels, variations in genetic makeups, and the amount and strain of virus that starts the infection.
As Dr. Fauci has explained, the reason many patients suffer the worst COVID-19 symptoms is because they have an immune system overreaction called a “cytokine storm.” In other words too much immunity can be worse than too little immunity. A “cytokine storm” is a sudden acute increase in circulating levels of different pro-inflammatory cytokines including IL-6, IL-1, TNF- a, and interferon. This increase in cytokines results in too many of them converging on the site of infection with destructive effects on human tissue. The damage to cellular interactions, vascular barriers, and capillaries can lead to multiorgan failure and ultimately death.
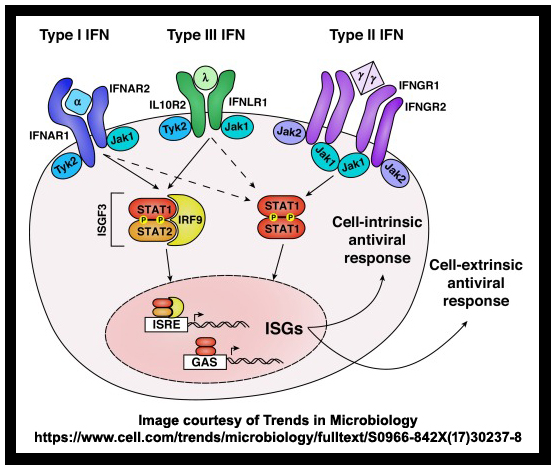
Recently, researchers discovered the role of a critical protein which could lead to a new potential COVID-19 treatment. Sibling studies comparing reactions to COVID-19 have revealed an interesting detail regarding the availability of interferon. Interferons are signaling proteins that help orchestrate the body’s defense against viral pathogens; they’re used to treat diseases like Hepatitis C.1
A growing body of evidence, including twin landmark studies recently published in the journal “Science” showed that “insufficient” interferon levels may be a dangerous precursor to a serious infection.2
“It looks like this virus has one big trick,” said Shane Crotty, a professor in the Center for Infectious Disease and Vaccine Research at the La Jolla Institute for Immunology in California. “That big trick is to avoid the initial innate immune response for a significant period of time and, in particular, avoid an early type-1 interferon response.”
The research highlights the potential for interferon-based therapies to expand a range of non-vaccine-related treatments, like Gilead’s Remdesivir and convalescent plasma. The timing of medical intervention is also critical.
“We think timing may be essential because it’s only in the very early phase one can really battle the virus particles and defend against infection,” said Alexander Hoischen, head of the genomic technologies and immuno-genomics group at Radboud University Medical Center in Nijmegen that analyzed the DNA of the two sets of brothers.
Then again, some people are believed to have trouble fighting infections because they make antibodies that deactivate their own interferon. Recently a global consortium of researchers said such immune reactions to the protein could account for life-threatening pneumonia in at least 2.6% of women and 12.5% of men that causes inflammation in the patient’s lungs.
Findings from the research offer the first explanation for the significantly higher mortality rate seen in male and elderly COVID-19 patients. According to the study published in “Science,” interferon-blocking antibodies appeared in 101 of 987 patients with severe disease, but none of the 663 people with an asymptomatic or mild case. Compared to younger patients, those over 65 were also more likely to have the autoimmune abnormality, which was “clinically silent until the patients were infected with SARS-CoV-2,” said the scientists. Consequently the researchers estimated that inteferon issues might underlie as many as 14% of fatalities and the most severe cases.
What these revelations point to is just another aspect of autoimmune disease. This is why protecting and strengthening natural immunity is so important. There are several diet and lifestyle tactics that are proven to improve immunity. The vast majority of Americans ignore most of them. That’s one of the big reasons why 18% of our nation’s GDP is for healthcare. That huge expense is also why many Americans demand that the government provide “free” healthcare.3
There are many thousands of studies that explain how Omega-3 essential fatty acids (EFAs) work with the immune system to make it function properly. They also show that inflammation is reduced significantly when the ratio of Omega-3 to Omega-6 EFAs is lower than 4:1 and preferably lower than 2:1 in the membranes of cells.4 5 6
Over the years I’ve written many columns about the importance of eating foods that boost natural immunity. The original diet of man did it in spades. It was only after man invented farming and could grow crops in abundance that were formerly scarce, did he start experiencing the inflammation and autoimmune issues that are so prevalent today.7 8 9 10
There is a long list of autoimmune diseases that can literally come and go depending on the foods consumed. A poor diet doesn’t impact everyone the same way because we all have different genetic makeups with inherited weaknesses. That’s why, while on the same diet, some people end up with rheumatoid arthritis and others may have asthma, multiple sclerosis, lupus, inflammatory bowel disease, diabetes, vitiligo, chronic inflammation, or psoriasis. And that’s just the short list!
The best foods are those that are nutrient dense and diverse, with close to 1:1 EFA balances, that are also low glycemic. Grass-fed meats, Omega-3 meats, wild-caught seafood, the dark green leafy vegetables, and many other vegetables such as squashes and beans are excellent selections. Foods high in Omega-6 EFAs should be avoided whenever possible. They are the seeds, nuts, grains, most oils, and grain-fed meats.11 12 13 14
If you want a strong immune system, diet is where you start. Then add in the following:
● Don’t Smoke
● Exercise Regularly
● Maintain a Healthy Weight
● Drink Alcohol Only in Moderation
● Get Adequate Sleep
● Minimize Stress and Anxiety
That formula works for everyone and will be the best protection you will ever have for viruses such as COVID-19 and influenza. It’s especially true for people over 65 years of age as the scientists have pointed out in regards to protecting against a severe reaction to a COVID-19 infection. It’s possible that old folks, like me, can be as safe as the youngsters. But we must be more proactive than they are by taking appropriate steps in improving our immunity in order to pull it off.
I provided this same advice regarding COVID-19 on February 21, 2020 in my first COVID-19 column titled “Coronavirus Immunity.” At that time COVID-19 was not yet called a pandemic and, according to https://www.worldometers.info/, there were just 365 reported cases and zero deaths in the US. (Although, it’s now believed that two deaths occurred in San Francisco’s China town in early February.) In the article I stated it takes about 10 weeks for most people to lower their high EFA ratios down to 4:1 or less. We’ve had plenty of time. Read my first article and you’ll see.15
Hey everyone, the only difference in my immunity advice in February is that we now know an autoimmune diet is even more important than we originally thought. Another difference, according to the CDC’s September 10, 2020 analysis, is that for younger citizens the fatality rate for COVID-19 is less than it is for influenza. We also know that hospitals are far better prepared, treatment protocols have improved significantly, and a vaccine is on the way. The issue I have with the vaccine is that historically, flu-like vaccines work best on younger citizens and not those who are older. So it may be best to take steps to improve your immunity and think of the vaccine as a backup measure.
To your health.
Ted Slanker
Ted Slanker has been reporting on the fundamentals of nutritional research in publications, television and radio appearances, and at conferences since 1999. He condenses complex studies into the basics required for health and well-being. His eBook, The Real Diet of Man, is available online.
Don’t miss these links for additional reading:
1. Interferon Type I from Wikipedia
2. Hidden Immune Weakness Found in 14% of Gravely Ill COVID-19 Patients by Meredith Wadman
3. Omega-3 Fatty Acids in Inflammation and Autoimmune Diseases by Dr. Artemis Simopoulos
4. Effects of Omega-3 Fatty Acids on Immune Cells by Saray Gutiérrez, Sara L Svahn, and Maria E Johansson
5. Omega-3 Fatty Acid and Glucocorticoid Additively Suppress Pro-inflammatory/ Interferon-Regulated Gene Responses and Inflammasome Activation in Novel Alveolar Macrophage Model by Lauren K. Heine, et al. from Federation of American Societies for Experimental Biology
6. The Importance of the Ratio of Omega-6/Omega-3 Essential Fatty Acids by A. P. Simopoulos, PhD
7. Immunity and You by Ted Slanker
8. Does Cholesterol or Inflammation Cause CHD? by Ted Slanker
9. We Need Inflammation, but . . . by Ted Slanker
10. Protecting Immunity by Ted Slanker
11. Omega 3 Test use slanker as an offer code and save
12. Ted Slanker’s Omega-3 Blood Test
13. Man Is an Extension of the Leafy, Green Plant by Ted Slanker
14. Food Analysis: EFA, Protein to Fat, Net Carbs, Sugar, and Nutrient Load by Ted Slanker
15. Coronavirus Immunity by Ted Slanker